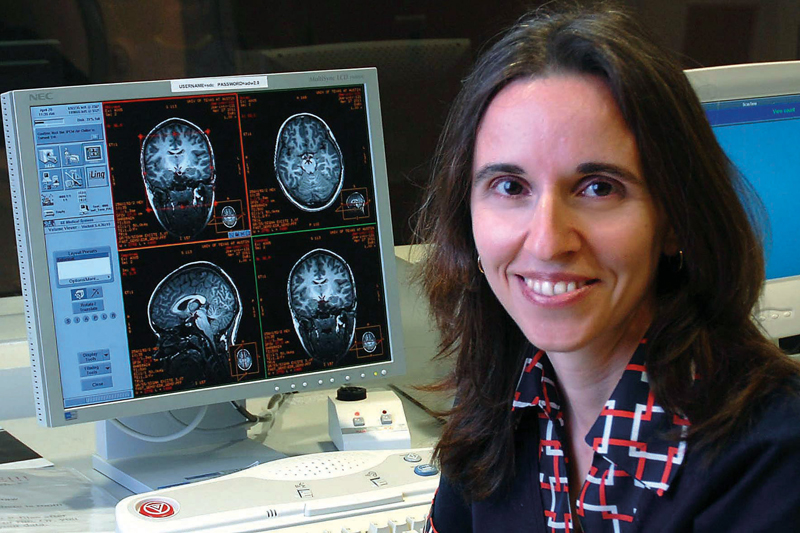
Psychology researcher Andreana Haley examines the link between dementia and obesity and aims to improve your brain’s health through diet and exercise
Step off the scale and let’s have a talk. You’re 30 pounds overweight and at risk for type 2 diabetes, hypertension, stroke, certain types of cancer and coronary heart disease.
More than 30 percent of Americans who are obese have likely endured a similarly uncomfortable conversation with their doctors during a routine checkup. Many are probably already familiar with the staggering list of diseases caused by their expanding waistlines but still can’t bring themselves to change their couch potato ways.
But what if dementia, a terminal disease that gradually erodes the powers of the mind, was also added to the list?
Findings from a recent brain-imaging study, conducted by Andreana Haley, assistant professor of psychology at The University of Texas at Austin, may add an extra incentive for middle-aged people to slim down. The study found impaired psychology insulin sensitivity, often caused by obesity, may have a direct connection to midlife brain vulnerability to cognitive decline.
“Very few people think of the brain consequences of obesity and the related metabolic dysfunctions,” Haley says. “I hope our research really drives home the point that to ensure successful cognitive aging for our rapidly growing elderly population, we need to investigate the mechanisms of early brain vulnerability.”
In search of early signs of brain vulnerability in middle-aged people, ages 40 to 60, Haley and her team of researchers compared brain response to a cognitive task among obese, overweight and normal-weight participants. They performed equally well on the tasks, which included exercises like remembering and manipulating numbers in short-term memory. However, obese and overweight individuals displayed a slower brain response in the inferior parietal lobe, a region in the brain that’s critical for planning and memory.
The researchers found the impaired brain activity may be a result of low insulin sensitivity, which causes the body to break down glucose less efficiently and derails blood oxygen flow to various regions of the body, including the brain.
In addition to memory loss, insulin resistance is associated with type 2 diabetes, an incurable disease suffered by 24 million Americans that can lead to kidney failure, amputation and blindness.
Haley says her research provides further evidence that a healthy lifestyle at midlife could lead to a higher quality of life later on, especially as people live longer.
According to the Centers for Disease Control and Prevention, average life expectancy in the United States has reached an all-time high of 78 years. But if people don’t take care of their health, their extended golden years may be filled with misery and debt.
Alzheimer’s disease, the most common form of dementia, costs the country $148 billion a year to provide care. But it also has a profound personal cost. The care needs of people with dementia, who progressively lose their memories and their personalities, are high and increase with time.
“Nobody knows what causes Alzheimer’s disease or other forms of dementia,” Haley says. “But it’s possible that this and other studies may show us ways that diet and exercise can be used to help prevent the onset of this disease or slow down the neurodegenerative process.”

Reclaiming the Brain
To determine if diet and exercise can slow down or perhaps even reverse the onset of dementia, the psychologists are now following up on their research with a 12-week exercise intervention study.
Partnering with researchers from the university’s Cardiovascular Aging Research Laboratory, Haley and her team are helping inactive adults learn the basics of eating healthy and working out. After a two-week fitness training session, the subjects are instructed to strap on a heart-rate monitor and walk about 45 minutes a day. Before and after the program, the researchers will analyze the respondents’ brain biochemistry and response to cognitive tasks.
Hirofumi Tanaka, director of the Cardiovascular Aging Research Laboratory and associate professor of Kinesiology and Health Education, says he hopes the fitness study will create awareness about the health risks of obesity and encourage a manageable means of prevention.
“Once you develop dementia, there’s no going back,” Tanaka says. “Prevention is the key, and exercise is the most promising strategy. To keep your brain healthy, you need to have good blood flow, and the way to have this is through exercise.”
The key to a long, healthy life is simple: eat right and exercise. But for many older adults who are set in their sedentary ways and busy with family and work obligations, adopting a new healthy lifestyle is easier said than done, Haley says.
According to a 2010 Gallup poll, more than 142 million American adults are overweight or obese. And nearly 60 percent would like to lose weight. But very few follow through with a long-term diet program, Haley says.
“It’s hard to motivate people by warning them about the long-term effects,” Haley says. “People still smoke even when they know they could develop cancer years later. But if we can show them how their brain improved after exercising and dieting for 12 weeks, maybe that’s the incentive they need to pursue a healthier lifestyle.”
A 60-year-old Austinite named Dan is well aware of the extreme life-threatening health consequences of obesity. At six-foot-one and 300 pounds, he suffers from myriad issues, including sleep apnea, hypertension and joint pain. He says he’s desperate to get his life back on track, but can’t find the motivation to lose the weight.
Although he has had “the weight talk” with his doctors for many years about the health risks of being too heavy, he still indulges in fried foods and sweet treats. Now diagnosed with type 2 diabetes, he says he knows he must change his ways or die.
Ashamed of his weight and weakened state of health, Dan requested his real name not be used in this story.
“I know I need to lose weight, but I can’t bring myself to do anything about it,” Dan says. “At this point, I lack the motivation to leave the house, let alone go to the gym.”
The 60-year-old Austin resident says the sleepless nights and chronic discomfort causes him to go through life in a disheveled daze, often forgetting mundane tasks like brushing his hair or picking up his prescriptions at the pharmacy.
“I’m open to the possibility that my brain is being affected by my weight,” Dan says. “Since I was diagnosed with type 2 diabetes five years ago, I’ve been experiencing more ‘senior moments’ than usual.”
Haley says more research needs to be done to figure out what exactly is responsible for the altered brain response observed in her study to determine the best treatment for people like Dan who can’t seem to win the battle of the bulge.
“Considering these people already show signs of altered brain function, the problem might be more than just weak will power,” Haley says. “There’s a possibility this damage is already affecting their ability to make changes in their lifestyle.”
Finding the Will to Change
So why has obesity become such a national problem? Why can’t people simply change their unhealthy habits and make the problem go away?
According to Russell Poldrack, professor of psychology and neurobiology and director of the university’s Imaging Research Center, the brain’s autopilot mechanism is to blame.
A leading expert in learning, memory and decision-making, Poldrack looks at what happens inside the brain when people try to un-learn bad habits. He says the brain’s autopilot is helpful because it takes control of all the thinking that goes into mundane daily rituals like driving to work or taking a shower. But if the daily ritual includes unhealthy habits like picking up a box of donuts on the way to the office, the autopilot can be a dieter’s worst enemy.
“The autopilot mechanism helps people go through the motions without overextending their cognitive resources,” Poldrack says. “But the mechanism can be very powerful when an unhealthy habit — like lighting a cigarette with your morning coffee — is already ingrained in your daily routine.”
Guilty pleasures like late-night snacking, smoking or impulsive shopping present a tradeoff between short-term gains and long-term pains, Poldrack says. And the short-term gains usually win.
“The immediate gratification of deliciousness and comfort that comes along with indulgences like eating a cupcake or taking a drag off a cigarette can trigger an overwhelming ‘let’s do it again’ message in the brain,” Poldrack says. “This overwhelming feeling can override a person’s goal to prevent cancer or lose weight.”
The key to avoiding the pull toward those guilty pleasures is to change the physical environment, Poldrack says.
“You have to realize that will-power is weak,” he says. “Make sure you don’t let yourself get into a situation where you have to overcome a bad habit. If it means stripping the pantry of all junk food or driving a different route to work to avoid the donut shop, you need to rearrange your habits to ensure your success.”
Philip Stanforth, lecturer in the Department of Kinesiology and Health Education and director of the university’s Fitness Institute of Texas, is familiar with the many obstacles overweight adults face when trying to lose weight. He says many of them get easily discouraged when they want to lose weight in a short time.
“There’s really no quick and easy way to lose weight and keep it off,” says Stanforth, who oversees fitness tests on students, faculty and staff, athletes and the public. “Rather than thinking about the long road to weight loss, they need to think more about the small steps they need to take. By thinking in baby steps, they’re more likely to stick with their diets and see the results.”
Today ’s Obesity Epidemic, Tomorrow’s Alzheimer’s Epidemic
Despite the increasing rates in obesity, Americans are living longer than ever. The Census Bureau predicts the nation will have more than one million centenarians by 2050.
The bad news is that healthcare costs are more than three times higher for people with Alzheimer’s and other forms of dementia than for other people age 65 and older, according to the Alzheimer’s Association.
“We can live long, but are we living to our fullest potential? Dementia has a huge social burden for the person who has it and for their caregivers,” Haley says. “Depression, apathy, withdrawal, loss of wages and the caregiver’s burden are all huge problems associated with the disease.”
According to the U.S. Centers for Disease Control and Prevention, Alzheimer’s disease affects about 5 million Americans and is the fifth leading cause of death in the United States.
“Findings from our study will not directly translate into new treatments,” Haley says. “But it gives us the potential to detect the brain vulnerability early on, and hopefully, we can do something about it.”